Opioid Substitution Therapy Works. India Isn’t Doing Enough
Epistemic status: Low-to-medium. This document is a shallow investigation on opioid substitution therapy (OST) access in India, focusing on buprenorphine
At Harvard Chan, We Need To Talk About Hard Things
Reposted from https://www.thecrimson.com/article/2025/10/31/narayanan-harvard-chan-school-funding-dialogue/ - Credits to The Harvard Crimson editors for supporting
We are all just animals. Why animal health is public health too
The vision of the Harvard T.H. Chan School of Public Health is bold - Health, Dignity, and Justice for
Breaking rules in hospitals - some advice
I love hospitals. I understand this is odd, but I feel safe in the cloud of phenol and Dettol in
Far too much love to give - navigating school, relationships & careers
I've been accused of the unthinkable. I've been called out. A dear friend and a beautiful
Transitioning from school to work is hard! Some advice on managing the self
Cross-post from the Effective Altruism Forum: https://forum.effectivealtruism.org/posts/b3DvgFscsp2ggd9P3/transitioning-from-school-to-work-is-hard-some-advice-on
I’m in graduate school now (MPH
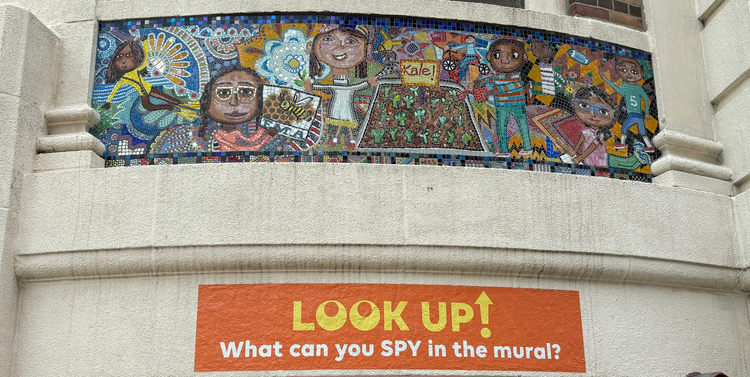
Day 4 in Boston
It's my 4th day in Boston, Massachusetts, and I'm wondering if I'll ever get
Failing to Protect India’s Children - Analysing State Capacity Deficits
With 444 million resident children, child protection forms a crucial part of India’s social development agenda. This is especially
Emotional risks in community work
Epistemic status: High - Built on experience, needs to be backed by more data
Reposted from https://globalhealthconnect.substack.com/
We're not teaching medicine well
A non-exhaustive list of reasons why medical education is currently failing in its mission to instil a rational and (therefore) people-centred mindset in practitioners.